Driving policy change to prevent maternal deaths
In 2009-12, 7.2 per 100,000 women died during or in the six weeks after pregnancy from medical and mental health causes compared with 3.5 women per 100,000 from obstetric causes.

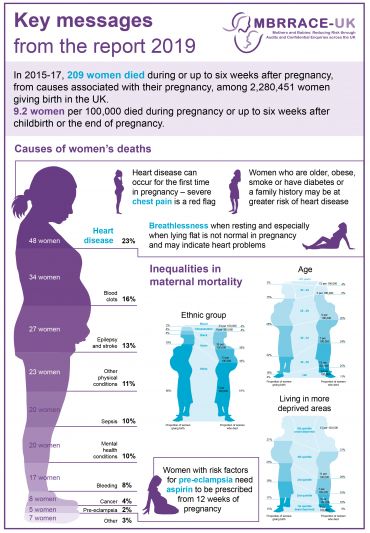
The research identified key areas where improved provision of obstetric medical care could prevent future maternal deaths and showed that 66% of the population attributable risk fraction of maternal death can be attributed to co-existing medical problems. Importantly, the research team also identified major inequalities in maternal mortality rates, such that black women were five times more likely, and Asian women two times more likely to die than white women.
The research team have introduced innovations throughout the programme to allow for the research to be translated more rapidly and effectively into policy change. These include development of a secure online reporting and assessment system, enabling expert health professionals from a wider range of specialties to identify improvements in care in parallel over a shorter time period than previously.
The work is cited as evidence underlying the national maternity strategy, including expanding access to specialist perinatal mental health services in the NHS England long-term plan published in January 2019, and new funding of £50 million for perinatal mental health services in Scotland, announced in March 2019.
The infographic in 2018 highlighting the ethnic disparities in mortality has completely changed the conversation around maternal health in the UK, sparking a widespread focus on addressing ethnic inequalities, including the ‘Five-times more’ campaign.
The MBRRACE-UK collaboration was appointed by the Healthcare Quality Improvement Partnership (HQIP)