Image credit: John Cairns
Revealing the brain's breathing secrets
'It became very hard to breathe…but I just had to remember to keep calm and still.'
You might be thinking that this sounds like a hapless victim from one of the increasingly ubiquitous Nordic noir dramas taking over our TV screens – so you may be surprised to learn that it's the experience of one of the subjects in a recent University of Oxford study! Olivia Faull and colleagues from the Oxford Centre for Functional Magnetic Resonance Imaging of the Brain (based in the Nuffield Department of Clinical Neurosciences) devised an experiment to look at what is happening in the brain when we might be about to become breathless. And the results have striking ramifications that will help us better understand – and may eventually lead to new treatments for –asthma and other chronic respiratory disorders.
Asthma costs the NHS £1bn a year, and the economy a further £2bn, due to time off sick (Asthma UK). It has long been suspected that some cases of asthma may be made worse by stress and worry. Sometimes breathlessness is out of proportion with what is actually happening physiologically in the lungs. In some people anxiety or worry can even bring on an asthma attack. Researchers in Oxford became interested in what is happening where in the brain when this reaction occurs.
A normal functioning PAG is clearly a good thing. We need to know when we are in danger, whether from something we could run away from – such as a hungry lion – or something we can't escape but could endure, such as becoming breathless. But what happens when things go wrong?
Scientists have known for some time that a tiny part of the brain called the periaqueductal gray (or PAG for short) plays an important role in how we perceive threat. Animal studies have revealed this bundle of cells in the brainstem to be the interface between automatic processes – such as breathing and heartbeat – and consciousness. The PAG is a group of cells ('grey matter') less than 5mm in diameter. Historically it has been very difficult to study in humans because it is so small and buried so deep. But the Oxford team managed to isolate the PAG using state-of-the-art magnetic resonance imaging (MRI) with super fine resolution.
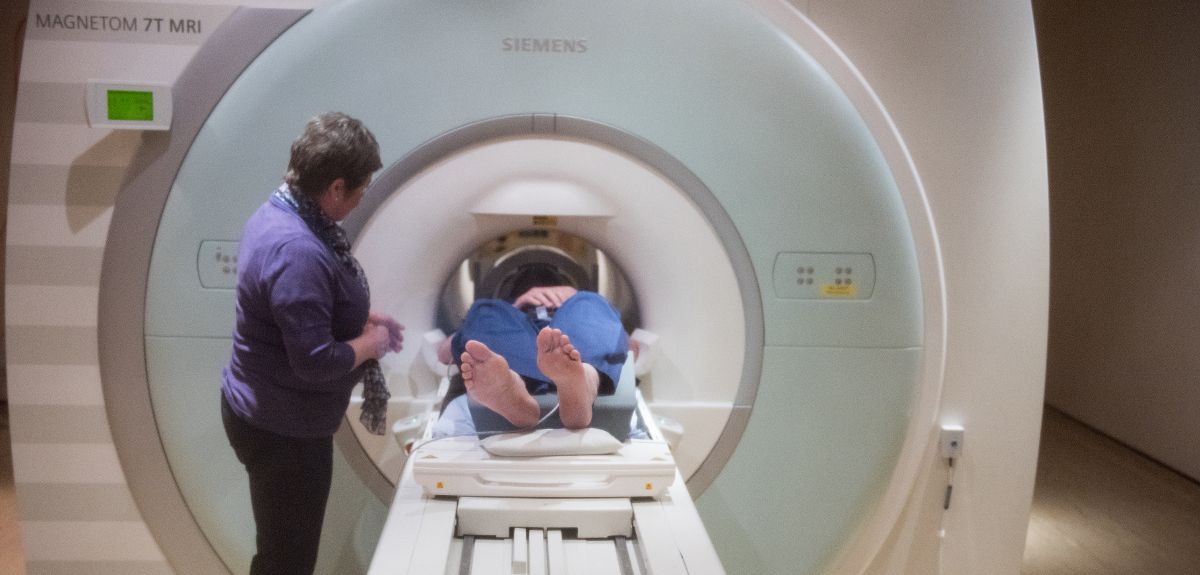
Olivia and colleagues scanned a group of healthy volunteers in the ultra high-field 7 Tesla MRI scanner. The volunteers wore a breathing system similar to a snorkel, that could be altered to produce a resistance when subjects breathed in (like breathing through a very narrow straw). During the scan, subjects looked at a screen that showed three different symbols at various times. Eventually the subjects learnt the meaning of the symbols – for instance the triangle meant that nothing would happen and they could breathe normally, and the star meant that their air would definitely be restricted and they would become breathless.
Volunteers therefore learned when they may be about to find it difficult to breathe. Olivia was then able to look at what was happening in the PAG both when people thought they might become breathless, as well as during the difficult breathing itself. Olivia wanted to know what was happening when people anticipate breathlessness, to better understand the stress and anxiety that exacerbate it. The study found that averaged over all participants, a particular subdivision of the PAG (called the ventrolateral column) became active when people anticipated that they might become breathless, and another subdivision (called the lateral column) became active while they were actually breathless. This means that different subdivisions of cells within the PAG are doing different things throughout the course of breathlessness.
A normal functioning PAG is clearly a good thing. We need to know when we are in danger, whether from something we could run away from – such as a hungry lion – or something we can't escape but could endure, such as becoming breathless. But what happens when things go wrong? It could be that in people who are hyper-sensitive to threats, the function of the PAG or its communications to the rest of the brain are altered. For example, some people with asthma may get very stressed if they can't find their inhaler, and this may even bring on an attack: perhaps the PAG is telling them that they are in danger of becoming breathless (even if, physiologically, at that moment they are breathing normally).
Now that this ground-breaking MRI experiment has enabled researchers to know where and how to look at the PAG, they can carry out further studies to find out more about asthma and other conditions where the physiology doesn’t match the perception – such as chronic pain or panic disorders. Such work could lead to the development of new treatments, to see whether they have any effect on this tiny, hitherto inaccessible part of the brain. These could be new medicines or new behavioural interventions such as as mindfulness or cognitive behavioural therapy, or combinations of both.
The full article is published in the journal eLife.