
Expert Comment: How can we address the nexus of climate change, migration, and infectious diseases?
The complex and intricate relationship between climate change, human migration, and infectious disease transmission presents an urgent global challenge, argues Dr Prathyush Sambaturu (Department of Biology, University of Oxford).
Climate change and its associated impacts have been closely linked to increased risks of infectious disease transmission, with projections indicating that these risks will further intensify the global burden of infectious diseases and lead to substantial disruptions in human societies. This situation is further complicated by a significant rise in the number of internally displaced persons (IDPs), which increased from 33.3 million to 71.1 million between 2013 and 2022, reflecting the extensive human displacement driven by various factors such as conflicts, violence, and natural disasters.
In a recent perspective piece in Nature Climate Change, our team of researchers — an international collaboration between researchers from the Department of Biology and the Pandemic Sciences Institute at the University of Oxford and Stellenbosch University’s Centre for Epidemic Response and Innovation (CERI) — came together to deepen our understanding of the impacts of the interrelated crises of climate change, migration, and infectious diseases and to explore their potential implications for research and policy. This work is part of the broader initiative to address the pressing concerns around climate-sensitive diseases as part of the Climate Amplified Diseases and Epidemics (CLIMADE) consortium.
Our review and analyses show that high-income countries that have contributed the most to global emissions face a lower infectious disease burden and are less vulnerable to the added impacts of climate change. On the other hand, low- and middle-income countries (LMICs) in Africa and Asia, that have made the least contribution to the global emission of greenhouse gasses, have continued to experience the greatest burden from infectious diseases and the highest vulnerability towards climate change. Most of the internal displacements as a result of weather-related hazards occurred in Asia and Africa.
Meanwhile, a large number of high-income nations, such as Portugal and Hungary, with high rates of outward migration are less vulnerable to climate change in comparison to the majority of low- and middle-income nations with high rates of inward migration such as Kenya and Uganda. This emphasizes the need for assessing the health effects of migration in low- and middle-income countries (LMICs) so as to ensure a more equitable approach to lowering the health effects of climate change. In recognition of the critical link between climate change and human health, COP28 for the first time introduced a dedicated Health Day, spotlighting clear, evidence-based pathways that illustrate how climate change directly affects human health.

We explore the specific pathways through which migration impacts infectious diseases. Migration, whether forced or voluntary, could alter the epidemiological landscape by introducing pathogens into new areas or by exposing migrants to diseases to which they have little or no immunity (acquired either through vaccination and/or exposure). The examples of Cholera and Hepatitis E outbreaks in refugee camps in Kenya, following severe droughts in the Horn of Africa in 2011, starkly illustrates how displacement can precipitate public health crises. These highlight the need for targeted interventions that address the vulnerabilities of displaced populations, particularly in LMICs.
To enhance the effectiveness of adaptation measures, it is essential to integrate climate risk assessments into national health planning, particularly in LMICs. This includes improving surveillance systems for infectious diseases, strengthening healthcare infrastructure, and ensuring that health facilities are resilient to climate impacts. Furthermore, the development and dissemination of early warning systems for climate-related health risks should be a priority.
Low- and middle-income countries in Africa and Asia, that have made the least contribution to the global emission of greenhouse gasses, have continued to experience the greatest burden from infectious diseases and the highest vulnerability towards climate change.
For instance, monitoring changes in disease vector populations and environmental conditions can help predict the spread of vector-borne diseases, allowing for pre-emptive actions to reduce transmission. We call for context-specific and multidisciplinary approaches to designing and implementing adaptation strategies to reduce the impact of migration on infectious disease spread. However, the implementation of these strategies remains a significant challenge, particularly in regions with limited resources.
In conclusion, our comprehensive analysis of the complex interplay between climate change, migration, and infectious diseases reiterates the urgent need for an integrated and equitable global response to these intersecting crises and to address the gaps in current approaches. The path forward requires a concerted effort to enhance global health security, promote climate justice, and build resilient communities capable of withstanding the dual threats of climate change and infectious diseases.
The perspective 'Impacts of climate change-related human migration on infectious diseases' has been published in Nature Climate Change.
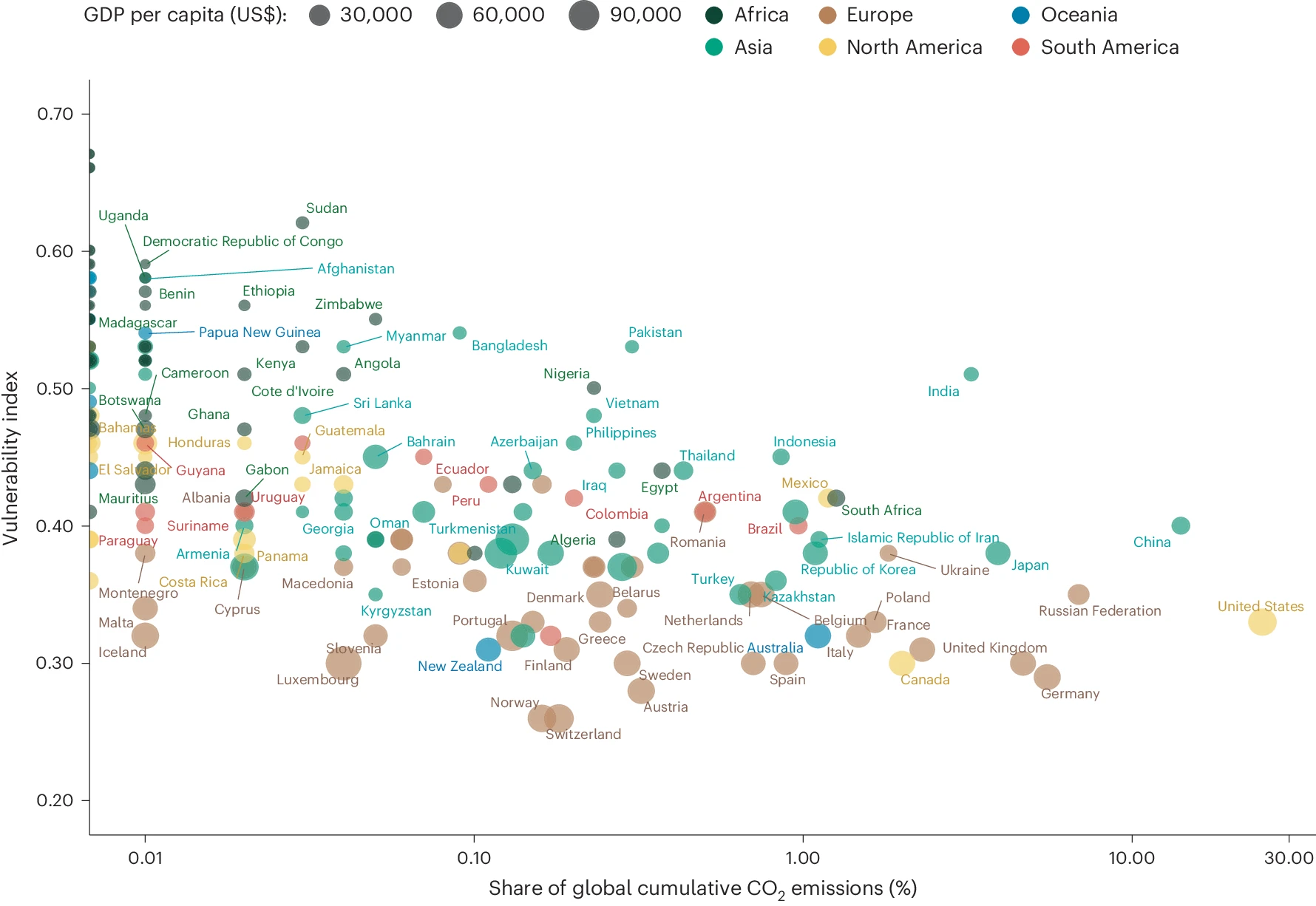
Share of global cumulative CO2 emissions and vulnerability index to climate change hazards per country. Points are coloured by continent, and size represents country GDP per capita in US$. Figure from Tsui, J.LH., Pena, R.E., Moir, M. et al. Impacts of climate change-related human migration on infectious diseases. Nature Climate Change. 14, 793–802 (2024).
 Cambridge victorious in Women's and Men's Boat Races 2025
Cambridge victorious in Women's and Men's Boat Races 2025
 Expert Comment: Ethical and legal challenges of uterus transplants in Mexico
Expert Comment: Ethical and legal challenges of uterus transplants in Mexico
 Oxford Humanities team delivers framework for tackling modern slavery and human trafficking
Oxford Humanities team delivers framework for tackling modern slavery and human trafficking
 Nearly 500,000 children could die from AIDS-related causes by 2030 without stable PEPFAR programmes, Oxford experts estimate
Nearly 500,000 children could die from AIDS-related causes by 2030 without stable PEPFAR programmes, Oxford experts estimate
 Exploring the health impacts of climate change
Exploring the health impacts of climate change
 Small temperature rise can cause large scale forced migration - study
Small temperature rise can cause large scale forced migration - study
 New multidisciplinary project will help forecast where and when deadly disease outbreaks are likely to occur
New multidisciplinary project will help forecast where and when deadly disease outbreaks are likely to occur