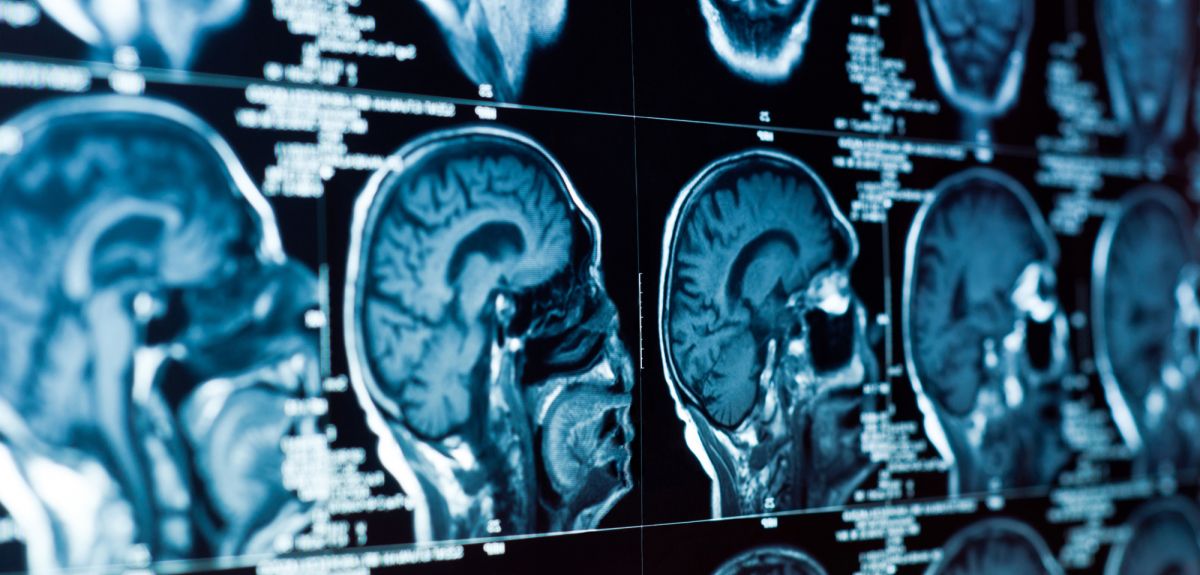
Poor metabolic health linked to worse brain health
People with poor metabolic health are more likely to have memory and thinking problems and worse brain health, according to a new study by researchers at Oxford Population Health. The study is published in Diabetes Care, and is the largest study into metabolic and brain health to date.
Poor metabolic health, also known as “metabolic syndrome”, is defined as having three or more of the following: a large waist circumference, high triglycerides, high blood pressure, high blood sugar, and lower levels of high-density lipoprotein (HDL) cholesterol, sometimes known as ‘good’ cholesterol. Globally, one in four adults live with metabolic syndrome.
Previous studies have shown that having poor metabolic health could increase the risk of developing dementia, but it was unclear whether it is linked to worse brain health even in people who do not have dementia. Maintaining both brain structure and cognitive abilities are crucial for healthy ageing as the loss of both can negatively impact brain health and might indicate progression towards dementia.
The researchers investigated whether having poor metabolic health affected brain volume and cognitive abilities by analysing results from 37,395 UK Biobank participants who did not have dementia; 7,945 of the participants had poor metabolic health when they joined the UK Biobank study.
The study found that having poor metabolic health was linked to:
• Lower total brain volume and lower grey matter volume, which is responsible for processing information in the brain;
• Increased white matter hyperintensities, a marker of vascular brain damage which has been previously linked to dementia;
• Memory problems, indicated by reduced hippocampal volume, and worse performance in cognitive tests of working memory (a type of short-term memory) and verbal declarative memory (ability to recall and repeat information);
• Worse performance in cognitive tests of processing speed (how quickly you process information), verbal and numerical reasoning (ability to understand and manipulate words and numbers), nonverbal reasoning (ability to understand information not presented as words or numbers, such as in pictures and diagrams), and tests of executive function (involved in planning and problem solving).
Danial Qureshi, PhD candidate at Oxford Population Health and lead author of the study, said ‘Our study findings show that poor metabolic health is associated with a reduction in brain volume and worse cognitive performance, and this may contribute to the future development of dementia. It is estimated that up to 40% of dementia cases may be preventable through dietary and lifestyle changes. Therefore, maintaining one’s metabolic health could be crucial for reducing the risk of dementia and related brain disorders.’
Dr Thomas Littlejohns, Senior Epidemiologist at Oxford Population Health and senior author of the study, said ‘Poorer metabolic health is thought to play an important role in future risk of developing dementia. Interestingly, our findings show that it is also associated with worse brain health even in individuals without dementia. These findings were consistent across different age groups, including those in their fifties, sixties, and seventies. The next step is to confirm if better prevention, treatment, and management of metabolic conditions leads to improved brain health in both mid and later life.’
Madeleine Walpert, Research Fellow at Dementia UK, said ‘This large study highlights the significance of recognising conditions that can increase dementia risk and exhibit similar symptoms to dementia. The findings show that metabolic syndrome reduces grey matter volume, increases vascular brain damage, and impacts cognition across domains like memory and processing speed – paralleling some hallmark symptoms of dementia.
This evidence reinforces the necessity of understanding how conditions interact and manifest with overlapping conditions, especially as 9 in 10 people with dementia also live with another long-term health condition. Treating and caring for people holistically, addressing not just individual conditions but also the interplay between coexisting conditions and their combined impact on overall health and wellbeing, is important.’
The researchers used data from the UK Biobank, which consists of more than half a million women and men who joined the study between 2006 and 2010 aged 40-69 years. From 2014 onwards, more than 50,000 participants underwent additional assessments, including brain imaging and completing a range of cognitive tests. Combining these data with other information is enabling scientists to provide unprecedented insights into how the diseases of ageing develop.
The study 'Association of Metabolic Syndrome With Neuroimaging and Cognitive Outcomes in the UK Biobank' is published in Diabetes Care.
 New study estimates NHS England spends 3% of its primary and secondary care budget on the health impacts of temperature
New study estimates NHS England spends 3% of its primary and secondary care budget on the health impacts of temperature
 International collaboration launches largest-ever therapeutics trial for patients hospitalised with dengue
International collaboration launches largest-ever therapeutics trial for patients hospitalised with dengue
 Oxford-built multi-agent assistant for cancer care to be piloted in collaboration with Microsoft
Oxford-built multi-agent assistant for cancer care to be piloted in collaboration with Microsoft
 World's first Phase II Nipah virus vaccine trial launch
World's first Phase II Nipah virus vaccine trial launch