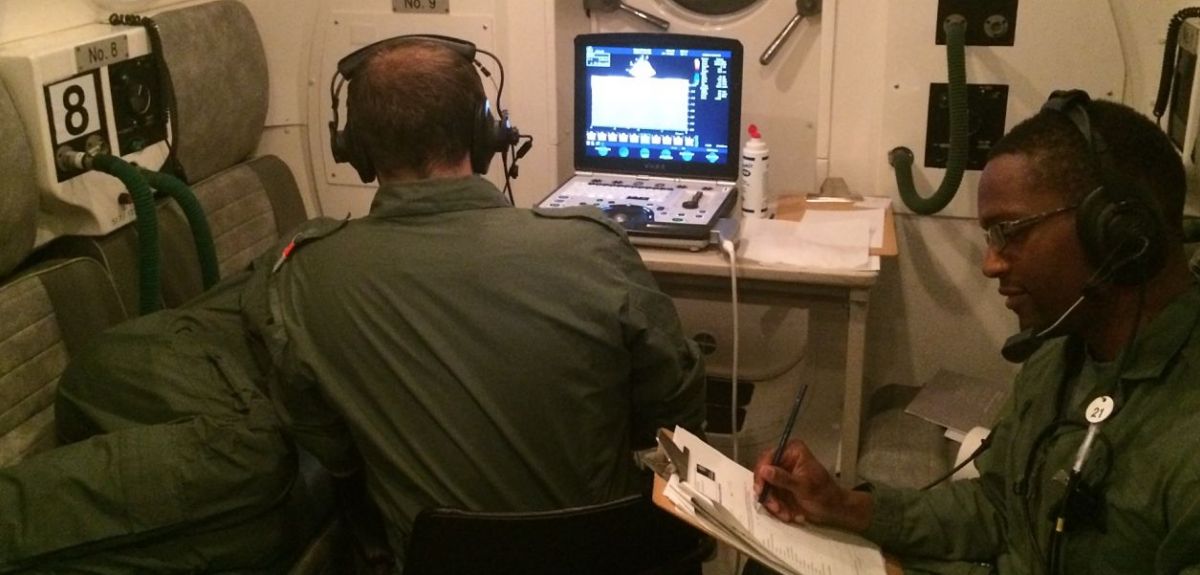
Image courtesy Dr Thomas Smith
Aviation study shows lower air pressure leads to higher blood pressure in the lungs
An Oxford University study has found that the lower-pressure environment experienced when flying increases blood pressure in the lungs. With an unknown but significant number of flights diverted each year for medical emergencies, the results could be used to improve health screening before flight as well as care for patients being moved by air.
Using a hypobaric altitude chamber, in which air pressure was decreased and increased to simulate the experience of a short-haul commercial flight, a team from Oxford's Aerospace Medicine Research Group, led by Dr Thomas Smith, monitored blood oxygen levels and pressure in the pulmonary artery, which carries deoxygenated blood from the heart to the lungs.
Dr Smith said: 'We already know that oxygen levels in the blood fall slightly during flights, but this study showed that pressure in the pulmonary artery increased in response to the reduction in oxygen. This was more noticeable in older people.
'Older passengers are more likely to require an aircraft diversion due to a medical emergency on an airline flight. It is too early to say if this effect could be behind some of those incidents, but we plan to do more research.’
In the study, healthy volunteers were placed in a hypobaric chamber at the Royal Air Force's Centre of Aviation Medicine. The air pressure was reduced to the equivalent of being at 6000 feet, then to the equivalent of 8000 feet, before being further reduced to the equivalent of 10,000 feet. The pressure in an airline cabin is normally maintained at a 5000 feet – 8000 feet level, which is why the study concentrated on the effect at that pressure. However, it is possible for private pilots to fly unpressurised aircraft up to 10,000 feet, and sometimes higher, without being required to use oxygen.
Dr Smith said: 'The effects we saw are not an issue for healthy passengers of any age. There may be increased risk for older passengers or private pilots who have an existing medical condition that increases pressure in the pulmonary artery or means that they are more susceptible to the effects of that increased pressure.'
Dr Smith, who is a specialist in transporting patients by air, added: 'These results also have implications for aeromedical transfers, when you want the patient to remain as stable as possible during a flight. For some patients on longer flights, it may be worth providing additional oxygen, even where that is not currently considered necessary. I have certainly changed my own practice in this regard.'
The team stress that further research is now needed to see if the results could be used to improve pre-flight medical screening and avoid more inflight emergencies.
 Expert Comment: Ethical and legal challenges of uterus transplants in Mexico
Expert Comment: Ethical and legal challenges of uterus transplants in Mexico
 Oxford Humanities team delivers framework for tackling modern slavery and human trafficking
Oxford Humanities team delivers framework for tackling modern slavery and human trafficking
 Nearly 500,000 children could die from AIDS-related causes by 2030 without stable PEPFAR programmes, Oxford experts estimate
Nearly 500,000 children could die from AIDS-related causes by 2030 without stable PEPFAR programmes, Oxford experts estimate